Informational purposes only, not medical or legal advice. Please consult your doctor or surgeon.
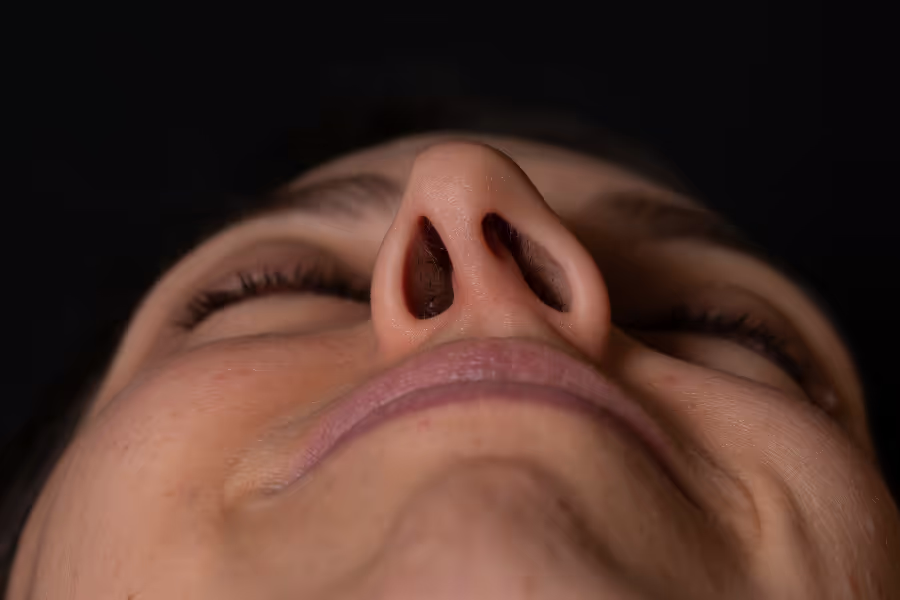
Septoplasty is surgery to straighten the wall inside your nose, called the septum. The septum divides your nose into left and right sides. If it’s bent (a “deviated septum”), airflow can be blocked, causing stuffiness, mouth‑breathing, snoring, nosebleeds, or trouble with sports and sleep. During septoplasty, the surgeon works through the nostrils—no external cuts—lifting the thin lining inside the nose to see the crooked cartilage and bone. They carefully reshape, trim, or reposition those parts so the septum sits in the middle and both nasal passages are more open.
Why do it? The goal is better airflow and easier nasal breathing, which can improve exercise tolerance, sleep quality, and how well sprays or allergy treatments work. Septoplasty focuses on function, not appearance. If someone also wants changes to the outside of the nose (like a hump or tip), that’s a different procedure called rhinoplasty; both can be combined as “septorhinoplasty” when needed.

Most septoplasties take about 60–120 minutes of operating time. Expect a few extra hours at the surgical centre for check‑in, anaesthesia, and recovery before you go home.
Check‑in and plan
Anaesthesia
Position and prep
Inside access (no outside cuts)
Straighten the septum
Stabilise
Rinse and check
Close up
Wake‑up and instructions

Every nose is different—follow your surgeon’s plan.
In Canada, private clinics charge between $5,000 to $12,000+.
In the United States, septoplasty can cost CA$4,500 to CA$30,000+ (the average being ~$13,500).
Exact prices depend on how complex your septum is, whether turbinate reduction is added, clinic location, and OR time. Many cosmetic clinics perform rhinoplasty + septoplasty (septorhinoplasty), which adds to the overall cost. Always ask for a written, itemized quote.
Choosing your surgeon is a benefit of pursuing private surgery. Here's how to make a wise choice.
Experience and volume
Credentials and training
Outcomes and safety
Indications and alternatives
Surgical plan and techniques
Facility accreditation
After‑care integration
Pricing transparency (private/self‑pay)
Special note on cosmetic clinics
Septoplasty is surgery to straighten the wall inside your nose (the septum) so air flows better.
No, you do not need a referral for a private septoplasty in Canada. You can book a consultation directly with a ENT surgeon, and they will review your options and diagnostics.
Your surgeon’s instructions come first—follow their plan if it differs.
Your personal risk depends on your health, how crooked your septum is, whether turbinates are also treated, the type of anaesthesia, and how closely you follow after‑care. Discuss your own risks with your ENT.
Septoplasty is generally safe and helps airflow for many people. Most issues are mild and short‑term; serious complications are uncommon, especially with careful after‑care and an experienced ENT.
Your situation depends on how blocked your nose feels day‑to‑day, what your exam/endoscopy shows (deviated septum, swollen turbinates, polyps), your allergy control, and how well non‑surgical care works (saline, steroid sprays, antihistamines). Talk specifics with your ENT.
Progressive symptoms and limits
Sinus and nose problems
Lower quality of life and performance
Medication dependence and side effects
Harder problem to treat later
If a crooked septum keeps you congested despite good medical care, delaying septoplasty can mean more mouth‑breathing, worse sleep, and recurring sinus issues. If symptoms are mild and controlled, careful non‑surgical management with regular check‑ins is a reasonable option. An ENT can help you decide which path fits your goals.
If you still have questions, then feel free to contact us directly.

Browse vetted ENT surgeons across Canada. Compare prices, qualifications, locations.
BROWSE SURGEONS