Informational purposes only, not medical or legal advice. Please consult your doctor or surgeon.
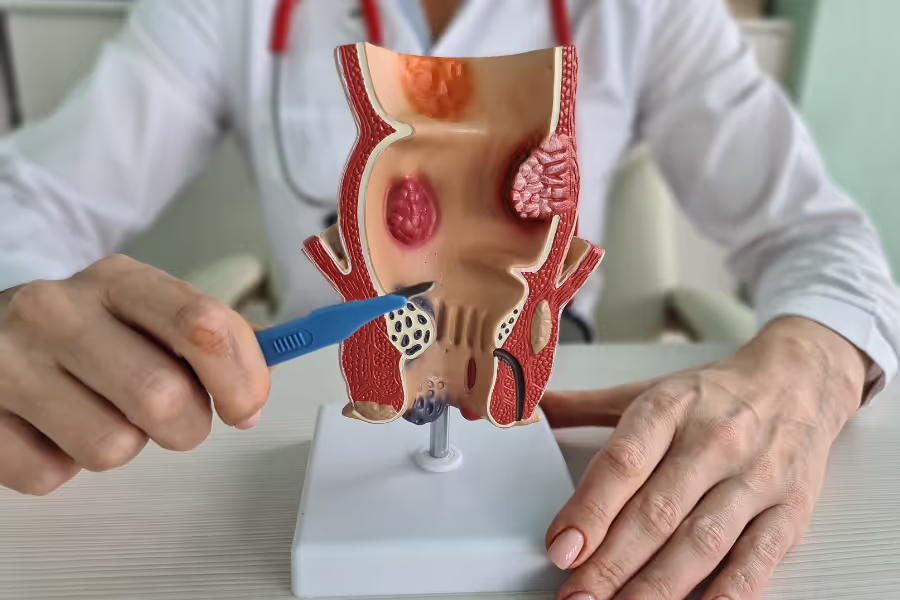
Hemorrhoid surgery is a procedure to treat swollen veins in the lower rectum or around the anus that cause bleeding, pain, itching, or lumps. When creams, fibre, or rubber band treatments aren’t enough, a surgeon can remove or shrink these veins so they stop bothering you.
There are a few ways to do it:

Most hemorrhoid surgeries take about 20–60 minutes. Plan a few extra hours at the centre for check‑in, anesthesia, and recovery before going home.
Basic steps

Every person heals differently—follow your surgeon’s plan. Taking the instructions seriously usually means a smoother recovery.
Week 1
Weeks 2–4
Weeks 5–8
Weeks 9–12+
In Canada, private clinics charge between $1,500 to $6,000 for hemorrhoid surgery. Higher end for multiple/external hemorrhoids, stapled procedures, or Doppler-guided/THD in premium facilities
Costs vary so much because of location, surgeon experience, facility type, complexity, and included services (some clinics offer all-inclusive, while others charge separately for anesthesia, followup care, etc.).
Choosing your surgeon is a major benefit of going private—use it to your advantage.
Hemorrhoid surgery isn’t for everyone, but it might be right for you if hemorrhoids keep bleeding, hurting, or prolapsing (bulging out) even after you’ve tried all the simpler stuff.
You’ve also tried conservative treatments without enough relief, like:
If those haven’t solved it—and symptoms are messing with school, sports, work, or sleep—surgery can remove or reduce the problem tissue so bleeding and prolapse stop. Talk to a colorectal or experienced general surgeon about your symptoms, what you’ve already tried, and which procedure (excisional, stapled, or Doppler‑guided/THD) fits your situation.
No, you do not need a referral for private hemorrhoid surgery in Canada. You can book a consultation directly with a surgeon, and they will review your condition, symptoms, and any previous treatments or diagnostics.
Your surgeon will give specific instructions—follow their plan first.
Your individual risk depends on your health, the type/grade of hemorrhoids, the procedure used (excisional, stapled, Doppler‑guided/THD), anesthesia, and how closely you follow after‑care. Discuss your personal risks with your surgeon.
Your situation depends on your symptoms (bleeding, pain, prolapse), exam findings (grade of hemorrhoids, internal vs external), your daily demands (school, work, sport), and how well non‑surgical care works (fiber, stool softeners, creams, banding). Talk specifics with your surgeon.
Progressive symptoms and life impact
Disease progression
Harder treatment later
Emergency evaluations
Quality of life and mental health
Medication-related downsides
If you still have questions, then feel free to contact us directly.

Browse vetted surgeons across Canada. Compare prices, qualifications, locations.
BROWSE SURGEONS

A highly specialized endocrine surgeon with 7 years of experience, offering expert management of thyroid & parathyroid disorders with a focus on minimally invasive techniques and patient-centred care.