
Informational purposes only, not medical or legal advice. Please consult your doctor or surgeon.
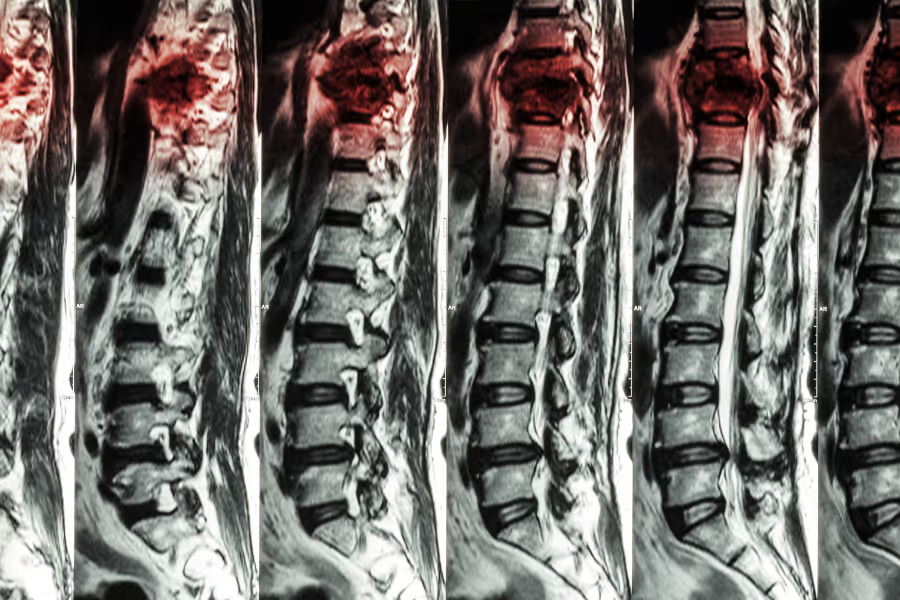
Kyphoplasty is a minimally invasive spine procedure used to treat painful compression fractures in the vertebrae (the building blocks of your spine). Imagine one of those blocks gets crushed down, often from osteoporosis or a hard fall. That collapse can cause sharp back pain and change your posture.
During kyphoplasty, the surgeon uses live X‑ray to guide a needle into the broken vertebra through a tiny skin puncture. Through this needle, a small balloon is slid into the bone and gently inflated. This can help lift the collapsed area and create a controlled space inside the vertebra. Once the space is shaped, the balloon is removed and the cavity is filled with a special bone cement. The cement hardens quickly, stabilizing the fracture from the inside so the bone doesn’t keep shifting.
Kyphoplasty doesn’t replace the whole vertebra; it reinforces the damaged part. The goal is simple: stabilize the crushed bone so movement hurts less, standing and walking feel more secure, and you can get back to everyday activities with better comfort.
Going private gives you more say in your care. You can:

Most kyphoplasty procedures take about 30–60 minutes per fractured vertebra of operating time. Add a few extra hours at the surgical centre for check‑in, anaesthesia, and recovery before you go home.

Every spine is different—follow your surgeon’s plan. The goal after kyphoplasty is to let the cemented bone settle while you slowly get your movement and confidence back.
Reality check: your back will feel sore at the puncture site, and you might be tired from anaesthesia.
Still annoying but usually much better than the original fracture pain for many people.
The “get your life back” phase.
Building strength and confidence.
Exact prices depend on how many vertebrae are treated, why they fractured, and whether you stay overnight. Always ask for a written, itemized quote.
In Canada, private clinics charge between $15,000 – $35,000.
In the United States, you can expect between CA$15,500 - CA$42,700.
Prices climb with more levels treated, extra cement, or if you need admission instead of same‑day discharge.
Choosing your surgeon/clinic is one of the biggest benefits of going private. Here's how to choose wisely.
Experience and volume
Credentials and training
Outcomes and safety
Indications and alternatives
Imaging and planning
Facility accreditation
Rehab integration
Transparent pricing
Kyphoplasty is a minimally invasive spine procedure where a surgeon stabilizes a crushed vertebra with bone cement.
No, you do not need a referral for a private kyphoplasty in Canada. You can book a consultation directly with a surgeon, and they will review your options and diagnostics.
Your surgeon’s instructions always come first—follow their plan if it’s different.
Stay moving (safely)
Quit smoking/vaping
Medications
General health
Medical clearance
Safe layout
Bed and bathroom
Comfort gear
Clothing
A helper
School and work
Travel
Meal prep
Pain and bowel plan
Fasting
Skin prep
What to bring
Your individual risk depends on your health, bone quality, how many vertebrae are treated, why they fractured (osteoporosis, cancer, trauma), anaesthesia, and how closely you follow instructions. Talk through your personal risks with your spine surgeon doctor.
Kyphoplasty is generally considered safe and can help many people with painful compression fractures. Most issues are mild and short‑term. The bigger worries are cement leakage, infection, blood clots, and ongoing pain if the fracture isn’t the only problem. An experienced spine team will explain which risks actually apply to you and how they’ll minimize them.
Your situation depends on how bad your pain is, how many vertebrae are fractured, what imaging shows (fresh vs old fractures, amount of collapse), your bone health (osteoporosis, cancer, trauma), and how well non‑surgical care is working (brace, meds, gentle movement). Always discuss details with your spine team.
(when pain from a compression fracture is significant and persistent)
Progressive pain and loss of function
Spinal collapse and posture changes
Breathing and fitness issues (with multiple fractures)
Lower quality of life and mood
Harder recovery later
Medication‑related harms
If you still have questions, then feel free to contact us directly.
Browse vetted spine surgeons across Canada. Compare prices, qualifications, locations.
BROWSE SURGEONS

Locally raised neurosurgeon specializing in minimal access neurosurgery and endovascular neurosurgery; with a clinical focus on cerebrovascular, spinal, and oncologic neurosurgery, and 21 years of experience.