Foreword
- Surgency is a platform that connects Canadians to private Canadian surgical providers. We do so in order to educate and empower Canadians who feel stuck on long wait lists. It is
- The following content is highly sensitive. It is not meant to fear-monger, or create false urgency to get surgery as fast as possible. It is meant to provide you with information. It should be helpful regardless of whether you ever intend to explore private surgical options.
- If you are worried about any of this subject matter, please consult your family physician who should be well equipped to let you know about your personal risks (if any).
Why Timing Matters for Knee Replacement
Timing matters. A Northwestern University study based on 8,002 participants suggests that 90% of patients with knee osteoarthritis who would likely benefit from knee replacement surgery aren't getting surgery soon enough, and benefitting less as a result. But at the same time, 25% of patients who don't need surgery are having it prematurely with little benefit.
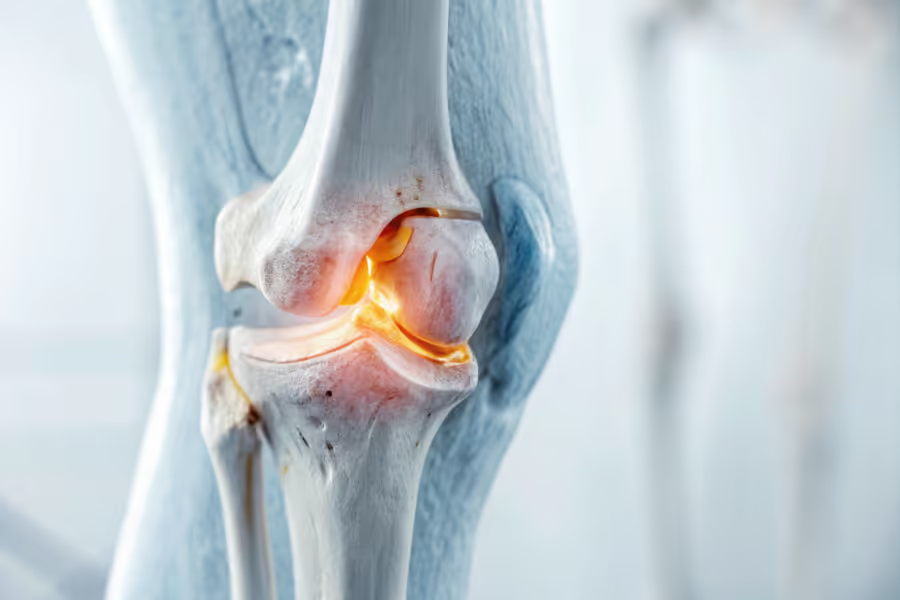
Most knee replacements are done because of osteoarthritis, a long-term, “wear and tear” condition. In simple terms:
- Smooth cartilage that covers the ends of the bones starts to break down.
- The space between the bones narrows.
- Movement becomes more painful and stiff over time.
This knee joint damage over time usually doesn’t reverse. Medications, injections, braces, and physiotherapy can help early on. But once the joint is badly damaged, these measures aren’t generally enough to keep you walking comfortably.
So when is the right time to consider surgery?
The goal is not to:
- Have surgery as early as possible, or
- Suffer until you can’t move at all.
Instead, good timing of knee replacement surgery usually sits at the point where:
- Pain is frequent and limiting,
- Everyday function (walking, stairs, work, chores, hobbies) is clearly affected, and
- X‑rays or scans show moderate to severe damage in the joint,
so that surgery is likely to meaningfully improve your quality of life.
A note on getting a surgeon's opinion:
If you are genuinely worried about your knee, and it is impacting your day to day, then you should try and get a surgeon's opinion. If you are struggling to get a surgeon's opinion in the public system, it can make sense to book consultations with one or more private surgeons for faster opinions (consults are usually within a few days). You'll need to pay $150-350 per consult, but the piece of mind might be worth it for you. Canadian surgeons are bound by strict ethical and legal duties (i.e. Canadian Orthopedic Association, Provincial College regulations), that prevent them from recommending unnecessary surgeries—even private providers.
You can book consults with private Canadian surgeons here.

What Are the Symptoms for Someone Needing a Knee Replacement?
Only a surgeon can confirm that a knee replacement is appropriate. But common symptoms that indicate you may need a knee replacement or at least a serious talk about one include:
- Severe knee pain most days, even at rest or at night
- Needing pain medication regularly just to get through ordinary tasks
- Difficulty walking, especially on uneven ground or longer distances
- Trouble with stairs, especially going down, or needing the railing for every step
- Struggling to stand up from a chair, couch, or toilet without using your arms
- Stiffness and limited range of motion, especially after sitting or first thing in the morning
- The knee “locking,” giving way, or feeling like it could buckle
- X‑rays or scans that show significant joint space loss, bone spurs, or deformity
If several of these apply, it’s a sign that conservative treatments may no longer be enough, and that it’s time for an in‑depth conversation about the risks and benefits of surgery—even if you’re not ready to book a date.
Immediate and Long-Term Risks of Delaying Knee Replacement
Some people hope that if they wait long enough, their knee will “settle down” or become tolerable. Unfortunately, osteoarthritis usually doesn’t work that way. With time, joint damage often gets worse, bringing new problems along with it.
Here is a simple snapshot of the trade‑offs:
Worsening Pain, Stiffness, and Joint Damage
When you delay knee replacement surgery for a long time, there is a material risk of:
- Cartilage breaking down. Less cushioning means more bone‑on‑bone contact.
- Pain ramping up from “activity only” to pain at rest and during the night.
- Knee changing shape. You might notice:
- Your leg looking more bowed or knocked inward
- Increased strain on ligaments
- Difficulty fully straightening or bending the knee
This deformity doesn’t just affect how it looks, it can:
- Make your walking pattern uneven
- Put more pressure on certain parts of the joint
- Limit future treatment options, including partial replacements or less invasive approaches
Loss of Mobility, Muscle Weakness, and Falls
When movement hurts, it’s natural to do less. Over months and years, this can create a cycle:
- Pain leads to less activity.
- Less activity leads to weak muscles, especially in the quadriceps and hamstrings.
- Weak muscles lead to instability and unsteady walking.
- Unsteady walking increases the risk of tripping or falling.
Falls can cause fractures, injuries, further loss of independence.
On top of this, people who arrive at surgery with very weak muscles and stiff joints often have:
- A harder time with physiotherapy,
- Slower gains in walking and stairs, and
- Higher risk of remaining stiff after surgery.
In other words, delaying can make recovery longer and more difficult when you eventually do have surgery.
Impact on Other Joints and Overall Health
Knee arthritis rarely affects only the knee in the long run. As you compensate for pain by limping or shifting your weight, other body parts can start to suffer:
- The other knee may develop arthritis faster because it is working overtime.
- Your hips, lower back, and feet can become painful from the uneven load.
- You may notice new issues like plantar fasciitis, hip bursitis, or back spasms.
Meanwhile, reduced activity affects your overall health:
- It becomes easier to gain weight, which adds even more strain to your joints.
- Blood pressure, blood sugar, and cholesterol can be harder to manage.
- Heart disease, type 2 diabetes, and sleep problems can worsen.
All of this can make future surgery more challenging and recovery less straightforward.
Quality of Life and Mental Health Consequences
Living with long‑term pain and limited mobility does not just affect your body. It can quietly change your entire life.
Many people:
- Start saying no to social events because standing and walking are too hard.
- Stop hobbies they once loved—gardening, golfing, travelling, exploring with grandchildren.
- Struggle at work or retire earlier than planned.
- Feel ongoing stress, frustration, shame, anxiety, or depression related to their knee.
Imagine a 72‑year‑old in British Columbia who used to walk the seawall with friends three times a week. As her knee worsens and her surgery date keeps getting pushed back, she gives up those walks, then coffee dates, then family trips. Her world shrinks, not because she wants it to, but because every outing feels like a risk.
How Waiting Affects Surgery, Recovery and Regret
More Complex Surgery and Limited Options
As knee damage advances, surgery can become technically more complex:
- There may be more bone loss to address.
- The deformity may be larger and harder to correct.
- The surgeon may need more specialized implants or longer operative time.
Patients who might once have been candidates for:
- Partial knee replacement, or
- Certain minimally invasive techniques
may lose those options if they wait until the joint is severely damaged. More extensive surgery can carry:
- Higher complication risk
- Longer time in the operating room and hospital
- More demanding rehab
This doesn’t mean every delay will lead to major complications. But it does mean that earlier, thoughtful decisions often leave more doors open.

Longer and More Difficult Rehabilitation
Your pre‑surgery baseline matters a great deal. A 2 year study of 222 patients undergoing hip replacement and knee replacement with worse baseline functional status (i.e. in relatively worse fitness/health), had worse function 2 years after surgery. Researchers concluded "performing surgery earlier in the course of functional decline may be associated with better outcome."
If you start from:
- Very poor range of motion
- Marked muscle weakness
- Low overall fitness
then rehab can feel like climbing a very steep hill.
You may:
- Need more sessions of physiotherapy
- Take longer to return to driving, work, and hobbies
- Be at higher risk of ongoing stiffness and pain
If your surgery date is still months away, there are steps you can take now:
- Ask about “prehab”: structured exercises and strengthening targeted to your legs, core, and balance.
- Discuss safe weight management strategies if relevant.
- Seek support for sleep, anxiety, and mood, which all affect how you experience pain and recovery.
These steps cannot erase arthritis. But they can turn a very steep hill into one that is at least manageable.
What Is the Regret Rate for Knee Replacements?
Research suggests roughly 10% of patients report dissatisfaction or regret, often due to ongoing pain, stiffness, or unmet expectations. When complications were excluded, that percentage dropped to 7.3%. Pain catastrophizing, pre-existing anxiety/depression, and coping skills were also cited as key indicators of dissatisfaction.
Here is what research and experience suggest:
- Most patients experience meaningful pain relief and better function after total knee replacement.
- A smaller group, around 7.3-10%, report dissatisfaction or regret.
Reasons for regret often include:
- Ongoing pain or stiffness, sometimes for reasons that are not fully clear
- Complications or infections
- A gap between what was expected and what was realistic
- Feeling that surgery was done too early, when symptoms were still tolerable
Regret is more likely when:
- Surgery is chosen before symptoms truly justify the risks.
- Patients are not fully prepared for the time and effort of rehab.
- Important mental health factors—such as strong fear of pain or high anxiety—are not addressed in advance.
The message is not to avoid surgery. Instead, it is to aim for clear, shared decision‑making:
- The right problem,
- The right procedure,
- At the right time—
with realistic expectations about what life will look like afterward.
When Is It Too Late for a Knee Replacement?
Many people in their 70s and 80s have successful knee replacements, but,
- the older and more medically complex someone is, and
- the more advanced the joint damage and deformity become,
the more careful surgeons must be about whether the benefits still outweigh the risks.
Situations where surgery may become less beneficial include:
- Severe deformity or bone loss that limits what surgery can reasonably fix
- Serious medical conditions (like advanced heart or lung disease) that make anesthesia very risky
- Very fragile health or significant cognitive decline, where active rehab would be difficult
- Multiple recent falls or fractures that suggest very unstable balance
Some red flags that it may be getting too late to keep waiting include:
- Frequent falls or near‑falls linked to your knee giving way
- Rapidly worsening knee shape (more bow‑leg or knock‑knee)
- Being unable to walk from room to room without major pain or support
- Needing hands‑on help for most basic daily tasks because of your knee
The “too late” question is best answered with an orthopedic surgeon who understands your full medical history, your imaging, and your personal goals.
When is it Too Early for Knee Replacement Surgery?
For younger patients (under 60), timing carries a different kind of risk. Operating relatively early,
- can improve quality of life sooner, but
- also increases the chance of needing a revision surgery later in life, and
- may raise the risk of regret if pain and disability were not yet severe.
In general, knee replacements are said to last 15-20 years. So if a 40 year old gets one, then the general understanding is they will likely need revision surgery at some point.
However, a recent 40 year study from Hospital for Special Surgery found that active, younger patients (40s - 50s) who received total knee replacements were unlikely to require revision in their lifetime.

How to Talk to Your Surgeon About Timing (and Avoid Unnecessary Delays)
Feeling unsure about when to move forward is normal. A clear, honest conversation with your surgeon can make a big difference.
Prepare Before Your Appointment
Consider bringing notes on:
- Pain patterns:
- When is your pain worst?
- What makes it better or worse?
- Activity limits:
- How far can you walk?
- How do stairs feel?
- What tasks are now impossible or exhausting?
- Treatments tried:
- Medications (and doses)
- Injections (and how long they helped)
- Physiotherapy or exercise programs
- Braces, canes, or walkers
Add a few reflective questions for yourself:
- “What daily activities am I no longer able to do because of my knee?”
- “If my knee were 50% better, what would I start doing again?”
- “How is this pain affecting my work, relationships, and mental health?”
Key Questions to Ask Your Surgeon
During your visit, you might ask:
- “What happens if I wait 6–12 more months?”
- “Do you think we are at the point where waiting is doing more harm than good?”
- “Would delaying knee replacement surgery change the type of surgery I might need later?”
- “What can I do now—prehab, weight management, mental health support—to improve my surgery outcome?”
- “Based on patients like me, what is a realistic expectation for pain, mobility, and the knee replacement regret rate?”
These questions help move the decision from “guesswork” to a shared plan.
Considering Faster Access Through Private Knee Surgery in Canada
For some Canadians, it may make sense to explore private options. At the very least, you can pay $150-350 to see a surgeon within a few days or weeks.
Public care usually still covers much of your ongoing health needs, such as family doctor visits, emergency care, and some imaging and rehab, depending on your province. Private surgery does not replace the public system—it complements it, especially when wait times feel unmanageable.
If you're curious about the cost of private knee replacement in Canada, you'll find this article helpful. If you would like to see vetted Canadian knee surgeons, then check out our directory.
Don’t Wait for Knee Pain to Decide for You
Delaying knee replacement surgery can:
- Allow joint damage, deformity, and pain to steadily worsen
- Shrink your daily world and independence
- Increase the risk of falls and other health problems
- Make surgery more complex and recovery more demanding
- Reduce the chance of the best possible outcome
At the same time, jumping into surgery too early can lead to disappointment and higher lifetime revision risk, especially in younger patients.
The safest path sits in the middle:
- Not ignoring the dangers of delaying knee replacement, and
- Not rushing before pain and disability truly justify the step.
If you’re in Canada and feeling stuck between long waitlists and worsening symptoms, remember:
- You are not alone in this.
- There are public and private options to explore.
- You deserve clear, honest information to make a decision that fits your life.
If you’re ready for a small next step, you might:
- Talk with your family doctor about your pain and function today, not just your X‑ray.
- Write down what you most want your knee to let you do again.
- Browse vetted knee surgeons in Canada on Surgency
You do not have to wait until your knee makes the decision for you.
FAQs: Risks of Delaying Knee Replacement Surgery
How long can I safely delay knee replacement if my pain is still manageable?
If pain is mild, your function is good, and conservative treatments are working, it may be reasonable to wait. However, if your walking distance is shrinking, you’re avoiding key activities, or your X‑rays show significant damage, waiting may allow joint damage and deformity to progress. The safe window is different for each person—review your symptoms and imaging with your surgeon regularly.
Does delaying knee replacement make recovery harder?
It often can. Longer delays usually mean weaker muscles, stiffer joints, and lower fitness by the time of surgery. All of these make rehab more challenging and can slow your return to normal activities. Prehab, gentle activity, and overall health management can help, but they can’t fully take away the impact of years of severe arthritis.
Are there risks to having knee replacement too early?
Yes. Having surgery while pain and disability are still fairly mild can:
- Increase the chance of regret,
- Raise the lifetime risk of needing a revision, especially in younger patients, and
- Leave you feeling that the trade‑off of risks and rehab was not worth it.
This is why the timing of knee replacement surgery should balance both sides: the well‑documented dangers of delaying knee replacement and the real downsides of operating before it is truly needed.
Medical Disclaimer:
This article is for general informational purposes only and does not provide medical advice, diagnosis, or treatment. Every patient’s situation is unique. Always consult a qualified healthcare professional, such as your family doctor or orthopedic surgeon, for advice about your own health and treatment options.




