
Informational purposes only, not medical or legal advice. Please consult your doctor or surgeon.
Vasectomy is a quick procedure that stops sperm from mixing with semen. Sperm travel through two tiny tubes called the vas deferens—from the testicles to where semen is made. In a vasectomy, a urologist makes small openings in the skin of the scrotum, finds each vas deferens, and then blocks them (by cutting and sealing, tying, or using clips). You still make semen and ejaculate normally, but it no longer carries sperm.
A vasectomy reversal reconnects those same tubes so sperm can travel again. Through small incisions, the surgeon uses a microscope to precisely stitch the cut ends of the vas deferens back together (vasovasostomy). If the pathway closer to the testicle is blocked, they may connect the vas deferens directly to the epididymis, the coiled storage tube where sperm mature (vasoepididymostomy). The goal is to rebuild a clear path so sperm can rejoin semen and potentially allow pregnancy with intercourse.
The wait time for a public vasectomy is usually under 1-2 months. But many men choose private options for speed relative to cost, as vasectomies range between $700 to $2,000.
Vasectomy reversals are not generally covered under public insurance, as they are considered elective, so must be done privately.

Takes about 10–30 minutes in a clinic (most are “no‑scalpel” with local numbing).
Basic steps
Surgery takes 2–4 hours (can be longer), done in an operating room with anesthesia.
Basic steps
Note: After a vasectomy, you’re not immediately infertile—you need a semen test later to confirm no sperm. Reversal aims to rebuild the pathway so sperm can mix with semen again.

Everyone heals differently—follow your surgeon’s plan. Taking the instructions seriously usually means a smoother recovery.
Week 1
Weeks 2–4
Key notes
Week 1
Weeks 2–4
Weeks 5–8
Your team will tailor specifics to you—when in doubt, ask before pushing activity.
In Canada private clinics charge:
In the United States, you can expect to pay:
Choosing your surgeon is a major benefit of going private—use it to your advantage.
Experience and volume
Credentials and training
Outcomes and safety
Procedure technique and equipment
Pre‑op evaluation and planning
Facility accreditation
Care pathway and follow‑up
Costs and transparency
Vasectomy and vasectomy reversal are opposite goals. One blocks sperm from joining semen (birth control). The other reconnects the pathway so sperm can flow again (to try for pregnancy). The right choice depends on your goals, health, and timeline.
No, you do not need a referral for a private vasectomy or vasectomy reversal in Canada. You can book a consultation directly with a urologist, and they will review your options and diagnostics.
Your urologist’s instructions come first—follow their plan if it differs.
Your individual risk depends on your health, anatomy, the exact technique (no‑scalpel vasectomy vs microsurgical reversal), anesthesia, and how closely you follow after‑care. Discuss your personal risks with your urologist.
60,000 Canadians get vasectomies every year. 2-6% of them will opt for a reversal.
Patency rates (i.e. sperm is present again in ejaculate) are 90-97% for vasovasectomy, and 80-90% for vasoepididymostomy.
But pregnancy ranges between 30-75%—depending heavily on the amount of time since the vasectomy.
If you still have questions, then feel free to contact us directly.

Browse vetted urologists across Canada. Compare prices, qualifications, locations.
BROWSE SURGEONS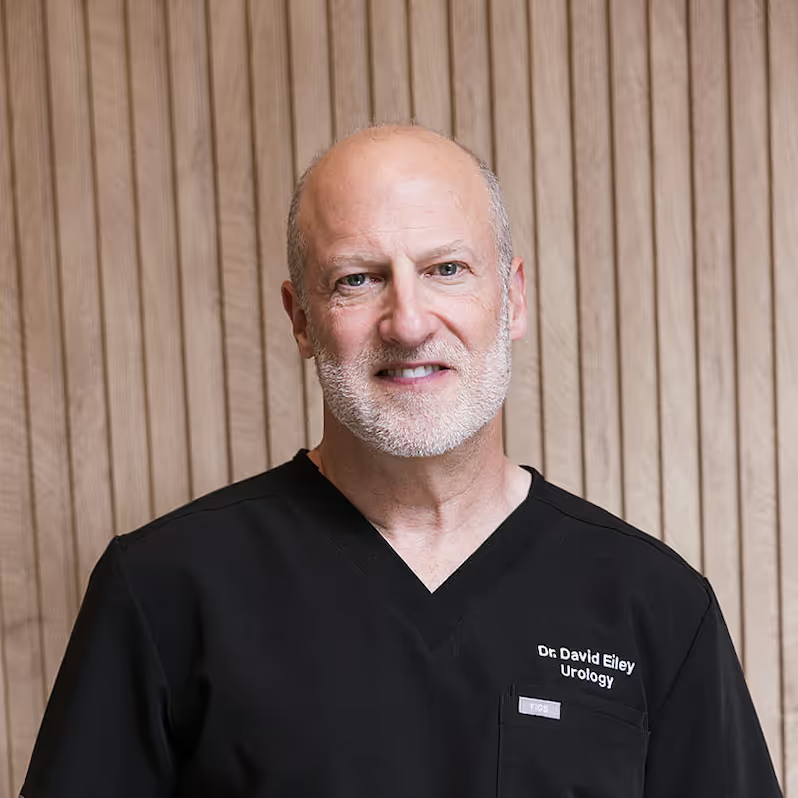

An FRCSC-certified urologist, with 25 years of experience, and 10,000+ procedures completed. Experienced with prostate disease, urinary incontinence, erectile dysfunction, bladder & testicular conditions.