Informational purposes only, not medical or legal advice. Please consult your doctor or surgeon.
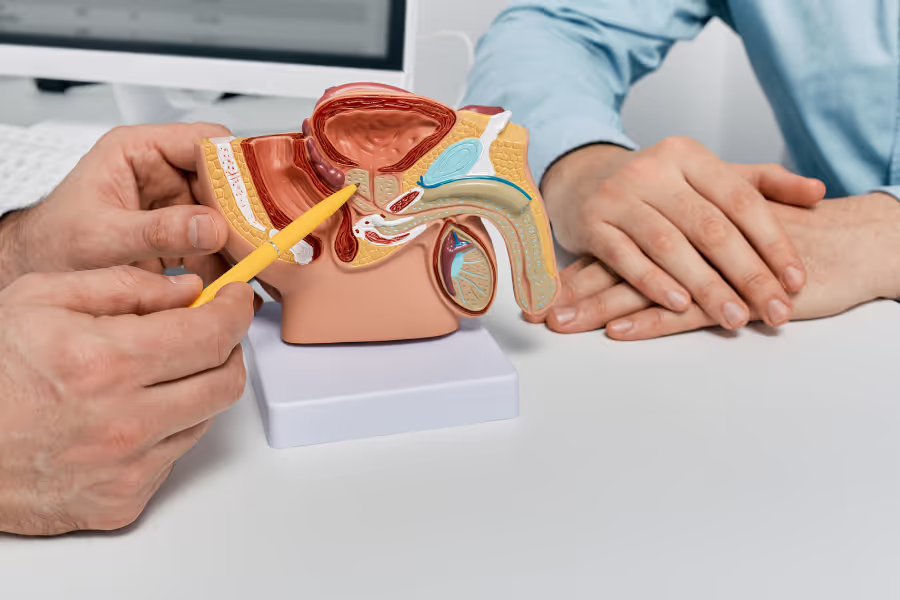
50% of men develop enlarged prostates (a small gland below the bladder). When this happens, it can squeeze the urethra—the tube urine passes through. This 'traffic jam' can cause a weak stream, urgency, frequent trips (especially at night), and the feeling you didn’t fully empty. It's a condition called benign prostatic hyperplasia (BPH). It's generally non-life threatening, but annoying and occasionally painful.
Before invasive procedures, many try medication (alpha‑blockers relax the channel; 5‑alpha‑reductase inhibitors shrink the prostate) and lifestyle changes (less evening fluids, caffeine moderation, timed voiding). These can reduce symptoms for many people and are often the first step.
TURP is a hospital procedure where a surgeon passes a thin camera through the urethra and trims away extra prostate tissue from the inside to widen the channel. No outside cuts are needed. Using an electric loop, the surgeon shaves tissue to open flow and improve emptying. It’s considered the classic “gold standard” because it directly removes the blockage. The amount removed is tailored to the prostate’s size and shape, aiming for a clear path from bladder to urethra and stronger, more reliable urination.
Rezūm uses controlled bursts of steam (heated water vapour) delivered through a small device inserted via the urethra. The vapour spreads into the enlarged prostate tissue, and the heat causes those cells to shrink over time. By reducing extra tissue volume, the urethral channel opens and urine can flow more easily. The treatment targets specific areas, including obstructing lobes, with brief injections of vapour. Because it doesn’t cut tissue, it focuses on making the prostate smaller from the inside to relieve pressure on the urinary pathway.
iTIND is a small, spring‑like metal device placed through the urethra into the prostate area for a few days. Its shape gently presses on the inside of the prostate and bladder neck, reshaping the channel to reduce blockage. After it’s been in place long enough to create these internal grooves, the device is removed through the urethra. The idea is mechanical remodeling from the inside to improve urine flow without permanently removing tissue, using the device’s expanding structure to “carve” a more open pathway.
Optilume uses a catheter with a balloon, inserted through the urethra to the tight prostatic area. When the balloon is inflated, it stretches the narrowed zone to create a wider channel. The balloon’s surface is coated with medication that helps limit tissue overgrowth where the stretch happened. After a short time, the balloon is deflated and removed. The combination of mechanical widening and localized drug delivery aims to keep the pathway more open so urine can pass more freely from the bladder.
UroLift places tiny permanent implants via a scope through the urethra. These implants act like curtain tie‑backs, pulling the enlarged prostate lobes away from the urethral channel to create an open corridor. No prostate tissue is cut out; instead, the tissue is held back to remove the squeeze on the urethra. The number of implants depends on the anatomy. By physically widening the passage, UroLift helps improve stream strength and emptying with a minimally invasive, internal “lift.”
Consult your physician or surgeon to see which option is right for you.

Your surgery/procedure may look different. Confirm with your urologist.
Surgery takes 60–120 minutes.
Basic steps
Procedure time ~10–20 minutes.
Basic steps
Placement takes ~5–15 minutes; removal ~5–10 minutes a few days later.
Basic steps
Procedures takes about 15–30 minutes.
Basic steps
Takes about 15–45 minutes.
Basic steps

Everyone heals differently—follow your surgeon’s plan. Taking instructions seriously usually means smoother results. Many clinics offer virtual check-ins.
In general, what to expect
Week 1
Weeks 2–4
Weeks 5–8
Week 1
Weeks 2–4
Weeks 5–12
Week 1
Weeks 2–4
Week 1
Weeks 2–4
Weeks 5–8
Week 1
Weeks 2–4
Weeks 5–8
Your team will tailor specifics to your prostate size/anatomy and the exact procedure—follow their instructions first.
Exact fees vary by province, clinic, device pricing, and complexity—always request a written, itemized quote.
In Canada, private clinics generally charge:
Choosing your urologist is a major benefit of going private—use it to your advantage.
Experience and volume
Credentials and training
Outcomes and safety
Indications and alternatives
Procedure plan and techniques
Imaging and planning
Facility accreditation
Experience and outcomes
Personalized fit
Peri‑operative plan
Logistics and costs
BPH procedures are options when an enlarged prostate is blocking urine flow and simpler steps aren’t fixing it. You might be a candidate if you have a weak stream, urgency/frequency (especially at night), trouble starting, stopping, or fully emptying, or you’ve had urinary retention, infections from poor emptying, bladder stones, bleeding from the prostate, or kidney strain.
In general, you should try meds and lifestyle changes first; if they don’t help enough or cause side effects, a procedure may make sense. Which one fits you depends on prostate size/shape, goals (like preserving ejaculation), and how fast you need relief.
No, you do not need a referral for private BPH surgery or BPH procedures in Canada. You can book a consultation directly with a urologist, and they will review your condition, symptoms, and any previous treatments or diagnostics.
Here’s a clear, practical guide to help you get ready for TURP, Rezūm, UroLift, iTIND, or Optilume. Your urologist’s instructions come first—follow their plan if it differs.
Your risk depends on your health, prostate size/shape (including a median lobe), the exact procedure (TURP, Rezūm, UroLift, iTIND, Optilume), anesthesia, and how closely you follow after‑care. Discuss your personal risks with your urologist.
Your situation depends on your symptoms (weak stream, urgency, nighttime trips), test results (flow test, residual urine, prostate size), and how well non‑procedure options work (meds, bladder training). Discuss specifics with your urologist.
Progressive symptoms and life impact
Bladder strain and damage
Urinary retention and emergencies
Infections, stones, and bleeding
Kidney risk
Harder treatment later
Medication-related downsides
If you still have questions, then feel free to contact us directly.

Browse vetted urologists across Canada. Compare prices, qualifications, locations.
BROWSE SURGEONS

An FRCSC-certified urologist, with 25 years of experience, and 10,000+ procedures completed. Experienced with prostate disease, urinary incontinence, erectile dysfunction, bladder & testicular conditions.

Leading urologist specializing in female pelvic medicine and reconstructive surgery. Her areas of expertise include pelvic organ prolapse, urinary incontinence (male and female), voiding disorders, BPH.