Informational purposes only, not medical or legal advice. Please consult your doctor or surgeon.
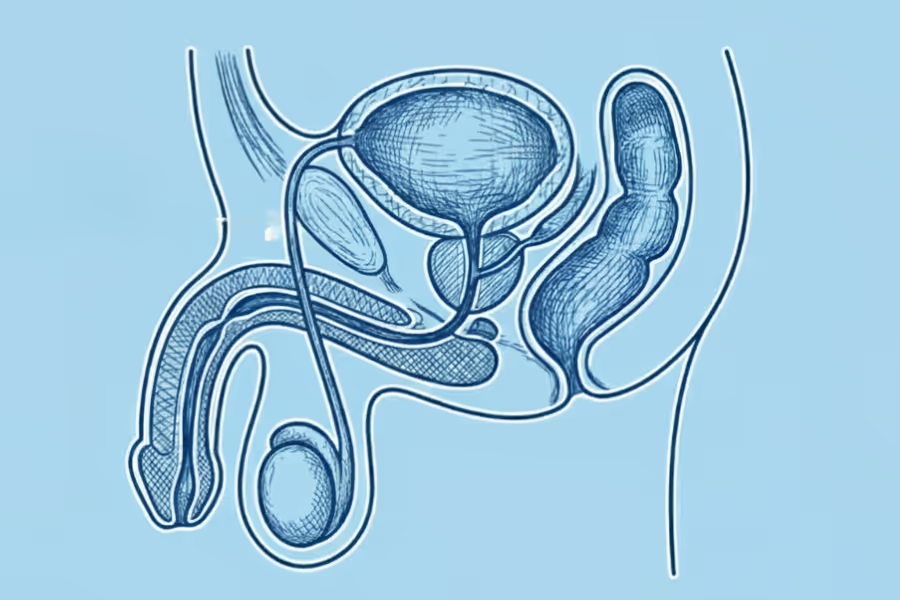
Urethroplasty is a surgery to fix a narrowed or blocked urethra—the tube that carries urine from your bladder out of your body. When this tube scars down (called a urethral stricture), the passage gets tight, and urine has to squeeze through a tiny space. That can lead to a weak stream, straining, taking forever to urinate, infections, or even urine backing up into the bladder.
In urethroplasty, the surgeon removes or opens up the scarred section and rebuilds the tube so urine can flow more normally again. Depending on how long and where the stricture is, your surgeon might:
The main goal is to give you a wider, stable urethra so urinating feels easier, more complete, and less stressful.
Procedure TypeWhat It InvolvesWhen It Is UsedExcision and Primary Anastomosis (EPA)The surgeon cuts out the entire scar tissue segment and then sews the two healthy ends of the urethra back together.Used for short strictures (typically 3 cm or less) where the ends can be reconnected without tension. High success rate (~95%).Augmentation Urethroplasty (Graft/Flap)The stricture is cut open, and a patch of tissue (a graft, most often taken from the inside of the cheek, called Buccal Mucosa) is sewn onto the urethra to widen its diameter.Used for longer, more complex strictures where removing the segment would make re-connecting the ends too tight.Staged UrethroplastyA complex repair done in multiple surgeries over several months.Used for very long strictures, severe trauma, or strictures caused by skin diseases like Lichen Sclerosus (LS).

Surgery usually about 2–4 hours, depending on how long the stricture is, where it is in the urethra, whether you need a graft. Expect to be in clinic most of the day for check‑in, anaesthesia, surgery, and early recovery.
1. Check‑in and planning
2. Anaesthesia
3. Position and prep
4. Accessing the urethra
5. Finding and opening the stricture
6. Graft (if needed)
7. Rebuilding the urethra and placing a catheter
8. Closing and dressing
9. Wake‑up and early recovery

Urethroplasty is a bigger surgery than a simple scope or dilation, so expect recovery to be a bit of a process. Everyone heals differently, follow your surgeon’s plan.
What it feels like
Main goals
Typical activities
What it feels like
Main goals
Typical activities
What it feels like
Main goals
Typical activities
What it feels like
Main goals
Typical activities
Anytime after surgery, contact your surgeon or go for urgent care if you have:
Recovery from urethroplasty is about being patient: protect the repair, respect the catheter, and follow your surgeon’s timeline, even if you feel better sooner.
For private care in Canada, urethroplasty is a major reconstruction, so it’s on the higher side. And the cost varies substantially based on the procedure type (excision and primary anastomosis, graft/flap, staged), location, surgeon expertise, anesthesia.
In Canada, private centres charge roughly $15,000–CA$30,000+
In the U.S., you can expect between CA$15,500 - $30,000+
Most bundled quotes typically cover:
These may be billed separately or handled outside the package:
Choosing your surgeon is one of the benefits of going the private route. Here's how to choose wisely.
Experience and volume
Credentials and training
Technique and tools
Outcomes and safety
Pre‑op and after‑care
Facility quality
Pricing transparency (for private care)
About the surgeon and plan
Anaesthesia and logistics
Recovery and follow‑up
Costs and documentation (if private)
A strong urethroplasty program is open about results, clear about the plan, easy to reach with questions, and totally transparent about what you’re paying for.
Figuring out if urethroplasty is right for you starts with what’s actually going on in your urethra, not just how annoying your stream feels. Your urologist will connect your symptoms, tests, and goals.
Common reasons people get urethroplasty:
No, you do not need a referral for a private urethroplasty surgery in Canada. You can book a consultation directly with a urologist, and they will review your options and diagnostics.
Your urologist’s instructions come first—follow their plan if it differs.
Your personal risk depends on your health, where the stricture is, how long it is, which urethroplasty technique is used, and how closely you follow after‑care. Your urologist will be in a better position to understand your personal situation.
These are uncomfortable but expected for many people:
These happen less often, but you should know about them:
Because urethroplasty is a reconstruction, there are some special considerations:
These are rare, but serious:
You can’t remove all risk, but you can tilt things in your favour:
Fever or chills, spreading redness or pus from the wound, catheter not draining, sudden trouble urinating, rapidly increasing swelling, severe pain that’s not controlled by meds, calf pain or shortness of breath. If these show up, contact your team or go to urgent care/ER.
Urethroplasty is a major but well‑established surgery. In experienced hands, most problems are mild and temporary, and the main goal is a more reliable, long‑term fix for your stricture.
Your situation depends on how bad your urinary symptoms are, what tests show (location/length of the stricture), your goals (comfort, avoiding catheters, long‑term fix), and how well simpler treatments work (dilations, temporary scopes, meds). Talk details with your urologist.
(when symptoms or tests are significant)
Progressive symptoms and limits
If the narrowing stays or worsens, you may have:
Some people end up needing repeated emergency visits for urinary retention (not being able to urinate at all).
Bladder and kidney strain
When urine can’t flow out properly, it can back up:
Harder problem to treat later
A long‑standing, untreated stricture can:
The longer abnormal urination patterns go on, the harder they can be to fully “reset,” even after surgery.
Quality‑of‑life drag
Living around a stricture can mean:
Over time, this can wear on mood, energy, and confidence.
Medication and short‑term fix downsides
Relying on repeated dilations or temporary procedures instead of a more durable repair can mean:
Delaying urethroplasty may be okay if:
You and your urologist should talk seriously about surgery if:
Urethroplasty isn’t for every minor narrowing. But if a significant stricture is repeatedly causing blockage, infections, or emergencies, timely reconstruction can protect your bladder and kidneys and make everyday life much easier.
If you still have questions, then feel free to contact us directly.

Browse vetted urologists across Canada. Compare prices, qualifications, locations.
BROWSE SURGEONS