
Informational purposes only, not medical or legal advice. Please consult your doctor or surgeon.
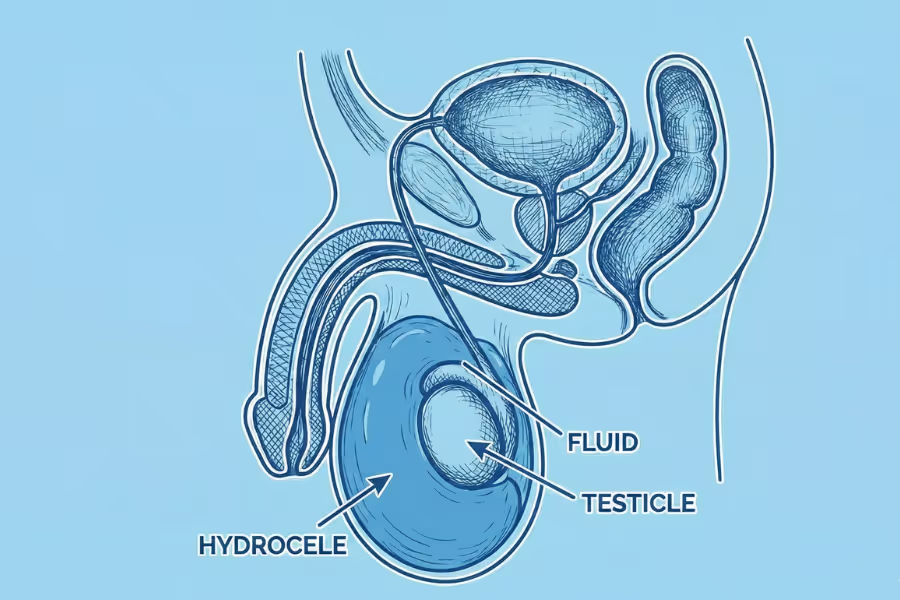
Hydrocele surgery is a procedure to fix a hydrocele—a buildup of fluid in the thin sac that surrounds the testicle. Think of it like a water balloon slowly forming around the testicle inside the scrotum. This extra fluid can make one side of the scrotum look swollen or feel heavy, and it may cause discomfort, especially with activity or at the end of the day.
During surgery, the goal is to drain the fluid and prevent it from coming back. There are two main approaches:
Hydrocelectomy: Through a small incision in the scrotum or lower abdomen, the surgeon opens the fluid‑filled sac, drains it, and either removes or reshapes the lining so fluid can't pool again.
Aspiration with sclerotherapy (less common): A needle drains the fluid, and a solution is injected to help seal the sac walls together. This is simpler but has a higher chance of the hydrocele returning.
Most hydrocelectomies are done as same‑day surgery under general or spinal anaesthesia. The aim is to get rid of the swelling, ease that heavy or achy feeling, and return the scrotum to a more normal size and comfort level.

Timings vary a bit by clinic and whether one or both sides are done, but here’s the general idea.
1. Check‑in and plan: You arrive, change into a gown, and meet the nurse, anaesthesiologist, and surgeon. They review your history and ultrasound, confirm which side(s) has the hydrocele, and answer last‑minute questions.
2. Anaesthesia: Most people get general anaesthesia, so you’re asleep and feel nothing. Some centres may use a spinal or local with sedation, depending on the case and your health.
3. Position and prep: You lie on a padded table. The scrotum and nearby skin are cleaned with antiseptic and covered with sterile drapes. The testicle is gently positioned so the surgeon can reach the hydrocele sac.
4. Incision and exposing the hydrocele: The surgeon makes a short incision in the scrotal skin over the swollen side. They carefully go down to the fluid‑filled sac around the testicle, protecting blood vessels and structures.
5. Draining and fixing the sac: The hydrocele sac is opened and the fluid is drained. Then, depending on the technique, the sac is either partly removed or turned and stitched in a way that stops fluid from easily collecting again.
6. Closing up: Bleeding is checked and controlled. The layers are closed with dissolving stitches, and a small dressing is placed. Supportive underwear or a scrotal support is usually put on to hold things in place.
7. Wake‑up and instructions: You wake up in recovery with nurses monitoring you. Once you’re stable, you get simple instructions about support, icing, activity limits, and pain meds, and you usually go home the same day with a ride.

Everyone heals a bit differently. Always follow your surgeon's plan. Hydrocele surgery is usually a same‑day procedure, but the area can be tender and swollen for a while.
Reality check: the scrotum often looks bigger, bruised, and feels tight or heavy. Walking can be awkward.
Still annoying, but usually improving.
This is the “steady” phase.
Most people are close to full comfort in daily life.
Overall, expect some bruising and weirdness at first, but with support, rest, and following instructions, most people are back to regular life over a few weeks.
Costs can vary a lot, so always ask each clinic for a written, itemized quote. Here’s a general idea.
Prices change by province, clinic, whether one or both sides are done, and how long the OR time is.
In the U.S., charges are usually higher once hospital and anaesthesia bills are included.
These parts may be billed separately or not covered in the package:
Getting to choose your urologist is one of the main benefits of going the private route. Hydrocele surgery is pretty routine, but you still want someone who does it well and runs an organized program.
A high‑quality program is open about results, clear on the plan, easy to contact, and fully transparent about costs.
Deciding on hydrocele surgery is about how much it bothers you, what the ultrasound shows, and what your goals are. Your urologist will help you determine if surgery makes sense.
If your symptoms and the ultrasound line up—and simpler stuff hasn’t solved the problem—hydrocele surgery can be a sensible next step. Your urologist can explain if now is the right time or if watchful waiting with check‑ins is safer.
No, you do not need a referral for a private hydrocele surgery in Canada. You can book a consultation directly with a urologist, and they will review your options and diagnostics.
Your urologist’s instructions always come first—if their plan is different from this, follow them. Think of this as a simple checklist to make surgery and recovery smoother.
Stop nicotine: Smoking/vaping slows healing and increases infection risk. Quitting 4+ weeks before surgery helps a lot.
Itemize your meds: Tell your team about every medication and supplement (prescriptions, Advil/ibuprofen, aspirin, vitamins, herbals). They may ask you to pause blood thinners, some anti‑inflammatories, or certain supplements that increase bleeding—only if your doctor says so.
General health: Light cardio (like walking), decent sleep, and balanced meals with some protein all make recovery easier.
Tests: Expect at least an ultrasound and bloodwork; other tests depend on your age and health.
Support gear: Have snug briefs or a jockstrap ready for 1–2 weeks after surgery, plus ice packs and loose sweatpants/joggers that fit over the dressing.
Bathroom: Stock gentle soap, clean towels, and a small bin or bag for used dressings.
Comfort zone: Set up a spot to rest with extra pillows (to support the scrotum/hips), easy access to water, your phone + charger, and your meds.
Ride and helper: Arrange a drive home—you cannot drive yourself—and try to have someone stay with you the first night.
School/work: Plan a few lighter days off. Avoid heavy lifting and intense physical jobs for a bit (your surgeon will give a timeline).
Travelling: If you’re coming from out of town, ask which follow‑ups can be virtual and how long you should stay nearby after surgery.
Fasting: Follow anaesthesia rules exactly (often no solid food after midnight, clear fluids only up to a set time).
Skin prep: Shower the night before and the morning of surgery. No lotions or powders near the groin. Don’t shave—your team will do any hair trimming if needed.
What to bring: Health card/ID, a list of medications, snug briefs or a jockstrap, and loose, easy‑on clothing for going home.
Your personal risk depends on your health, how big the hydrocele is, whether one or both sides are done, the exact technique your surgeon uses, and how closely you follow after‑care. Go over your own situation with your urologist.
These are the things most people notice:
These happen less often, but you should know about them:
These are rare, but more serious:
You can’t make risk zero, but you can tilt the odds your way:
fever or chills, spreading redness or pus, rapidly growing swelling, scrotum that suddenly feels rock‑hard and very painful, trouble urinating, calf pain, or shortness of breath. If these show up, contact your team or go to urgent care/ER.
Hydrocele surgery is a routine operation with a good safety record in experienced hands. Most side effects are mild and short‑lived; serious complications are uncommon.
Your situation depends on how big the hydrocele is, how much it actually bothers you, what the ultrasound shows, and what your goals are (comfort, confidence, sport, etc.). Talk specifics with your urologist. Here’s the general picture.
(when symptoms or size are significant)
A hydrocele is basically a “water balloon” of fluid around the testicle. If it keeps growing or staying big:
If you’re always using anti‑inflammatories or painkillers to “get by” instead of dealing with the root problem:
You and your urologist should talk seriously about surgery if:
Hydrocele surgery isn’t urgent for everyone, but if the swelling is big, persistent, and messing with your life, fixing it sooner can improve comfort and confidence and reduce the need for constant work‑arounds.
If you still have questions, then feel free to contact us directly.
Browse vetted urologists across Canada. Compare prices, qualifications, locations.
BROWSE SURGEONS

An FRCSC-certified urologist, with 25 years of experience, and 10,000+ procedures completed. Experienced with prostate disease, urinary incontinence, erectile dysfunction, bladder & testicular conditions.