
Informational purposes only, not medical or legal advice. Please consult your doctor or surgeon.
Bladder stone removal surgery is a procedure that gets rid of hard mineral stones sitting inside the bladder. Bladder stones can form when urine doesn’t empty fully and leftover urine concentrates into crystal clumps. Over time, those crystals can stick together and turn into a stone that irritates the bladder or blocks urine flow.
Most bladder stone removal is done with a small camera called a cystoscope. The urologist passes the scope through the urethra into the bladder, so there are no outside cuts. Once the stone is found, the surgeon breaks it into smaller pieces using energy (often a laser or ultrasound tool). Then the fragments are washed out or removed with tiny graspers through the scope.
In some cases—usually if the stone is very large or the anatomy makes scope access difficult—removal can be done through a small incision into the bladder instead. The main goal is simple: clear the bladder of stones so urine can flow normally again.
Canadians usually choose private bladder stone removal for the same reason people go private for many procedures: time, control, and fewer repeat crises. Your best option depends on symptoms, stone size, and whether there’s an underlying blockage (like BPH) causing poor emptying.

How long bladder stone removal takes depends mostly on stone size/number and whether it’s done with a scope (most common) or through a small incision (less common).
Most common (scope removal: cystolitholapaxy)
Less common (open or small‑incision bladder stone removal)

Everyone heals a bit differently, so your surgeon’s instructions come first. Bladder stone removal is usually a scope procedure, so recovery is often faster than “big” surgery, but your bladder can feel irritated for a while.
What it feels like
Main goals
Typical activities
What it feels like
Main goals
Typical activities
What it feels like
Main goals
Most people feel noticeably better as the bladder lining calms down and the irritation from the stone and instruments settles.
Pricing depends on stone size/number, whether it’s done by scope (most common), what anaesthesia is used, and whether you need extra procedures (like treating a blockage at the same time). Always ask for a written, itemized quote.
For a typical scope procedure (cystolitholapaxy / cystoscopic bladder stone removal), Canadian private centres charge: $6,000–CA$12,000+
If it’s a very large stone or requires a more complex approach (or longer OR time), costs can be higher.
In the United States, total charges can be higher: CA$7,000–CA$20,000+
Most bundled/private quotes typically include:
These are commonly separate or outside the package:
Choosing your surgeon is one of the biggest benefits of going private—here's how to use it to your advantage.
A good clinic should review your imaging and itemize:
Ask how they plan to remove the stone:
Ask for practical, real‑world numbers:
The best clinics don’t just remove the stone—they connect the dots:
A high‑quality bladder stone program is organized, transparent, high‑volume with scopes, and has a clear plan to remove the stone and deal with the reason it formed.
Bladder stone removal surgery is when a urologist uses a small scope (camera) through the urethra to break up and remove stones sitting in the bladder.
Don’t wait at home if you have:
A simple way to think about it: if a bladder stone is causing blockage, bleeding, infections, or repeated major symptoms, removal is often the most direct fix. If it’s tiny and quiet, monitoring may be reasonable.
No, you do not need a referral for a private bladder stone removal in Canada. You can book a consultation directly with a urologist, and they will review your options and diagnostics.
Your surgeon’s instructions come first—follow their plan if it differs. Bladder stone removal is usually done with a scope through the urethra, so prep is mostly about safety (infection/bleeding risk) and smooth logistics.
Depending on your age and history, the clinic may itemize:
Your individual risk depends on your health, the size/number of stones, whether you have an infection, the approach used (usually a scope through the urethra), and the type of anaesthetic. Your urologist should explain what applies to you.
Many people have mild, short‑term irritation and do well. The serious risks are uncommon, especially with an experienced team and good pre‑op infection screening.
Whether it’s safe to delay depends on your symptoms, stone size/number, whether you’re getting infections, and why the stone formed (often poor bladder emptying). Your urologist can match the plan to your scans and your health.
Bladder stones often happen because urine isn’t emptying well (for example BPH, urethral stricture, neurogenic bladder, catheter use). If the stone stays, the cycle often continues.
If you still have questions, then feel free to contact us directly.

Browse vetted urologists across Canada. Compare prices, qualifications, locations.
BROWSE SURGEONS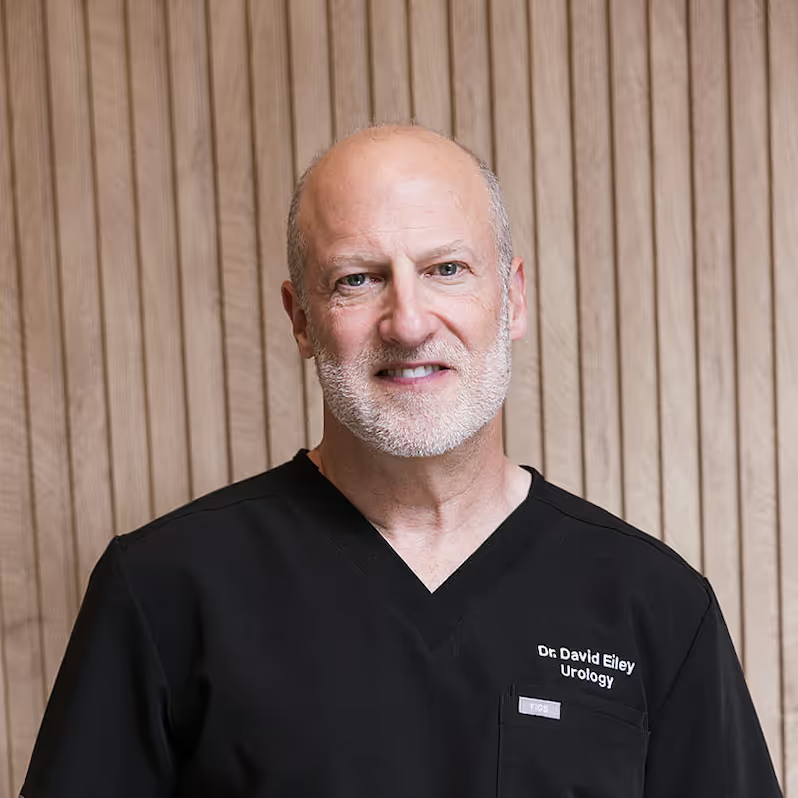

An FRCSC-certified urologist, with 25 years of experience, and 10,000+ procedures completed. Experienced with prostate disease, urinary incontinence, erectile dysfunction, bladder & testicular conditions.